Medicinal Plants in Dermatology: Salicylic Acid
Learn about the history, composition, and modern applications of a scientifically proven plant-derived therapy for skin conditions.

This post is part of a series where I break down the topics covered in our recently published review article on plants used in dermatology. Today, we’re covering Salicylic Acid (SA).
Israyilova, A., T.V. Peykova, B. Kittleson, P.C. Sprowl, T.O. Mohammed, C.L. Quave. (2025) From Plant to Patient: A Historical Perspective and Review of Selected Medicinal Plants in Dermatology. JID Innovations, 5:1: 100321
Discovery and Composition
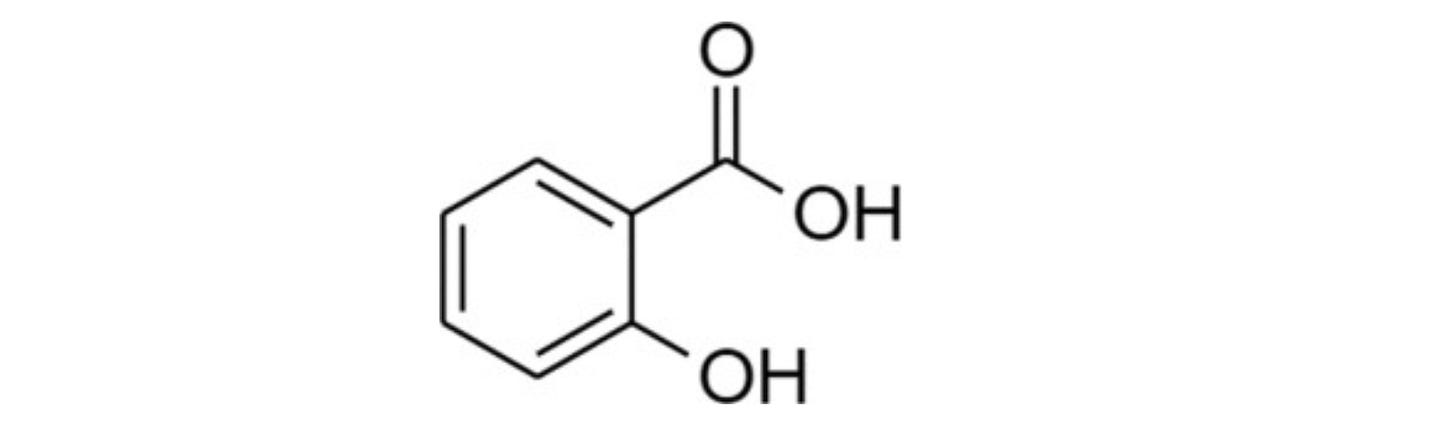
Salicylic acid (SA) is a natural compound found in willow bark, birch, meadowsweet, and wintergreen leaves. It consists of a benzene ring with carboxyl and hydroxyl groups. Salicin, its active component, was first extracted in the early 1800s and later refined, leading to the creation of aspirin (acetyl salicylic acid), a widely used anti-inflammatory and pain-relieving drug.
History as a Drug
Salicylic acid (SA) has been used for over 2,000 years to treat skin conditions and as a pain reliever. The ancient Greek physician Hippocrates recommended willow bark for pain and fever, and Roman naturalist Pliny the Elder used it for calluses. In 1757, Reverend Edward Stone rediscovered willow's medicinal properties. By 1824, salicin was extracted from willow bark, and in 1838, its molecular formula was identified. SA’s exfoliating effects on the skin’s outer layer were noted in the 1860s, and in 1882, dermatologist Paul Gerson Unna highlighted its chemical peeling benefits. Later, German chemist Felix Hoffmann modified SA to create aspirin in 1897. Today, SA is a key ingredient in creams, gels, and cleansers, primarily for treating acne by promoting skin cell renewal.
Mode of Action
SA works by dissolving the bonds between skin cells, promoting exfoliation and the removal of the skin’s outer layer. It targets proteins called desmosomes, which help cells stick together, making the skin easier to shed and renew. While early studies suggested SA didn’t affect skin thickness, recent research showed a 30% SA peel increased epidermal thickness and improved acne by enhancing the skin’s microenvironment. Widely used in over-the-counter acne treatments, SA is found in products with concentrations of 0.2–5%, highlighting its popularity and versatility in skincare.
Uses in Dermatology Today
Salicylic acid (SA) is a key ingredient in over 80 topical treatments for skin conditions like acne, warts, melasma, and ichthyosis. Widely available in over-the-counter products such as cleansers, creams, and serums, SA is also used in prescription-strength forms for more intensive care. Its exfoliating properties help remove dead skin, enhance absorption of other skincare treatments, and boost the effectiveness of medications like corticosteroids for psoriasis. However, improper use can lead to irritation, allergic reactions, or systemic toxicity, so it’s important to follow instructions and consult a healthcare provider when needed.
Acne
Acne affects about 10% of people, ranging from mild comedones to severe cysts. SA is a popular topical treatment due to its antibacterial, anti-inflammatory, and pore-clearing properties. One study found that a 30% SA peel reduced acne-causing bacteria and inflammation, including redness, by lowering levels of proinflammatory cytokines. These findings highlight SA’s effectiveness in managing moderate-to-severe acne and regulating the skin microbiome.
Warts
Warts are harmless skin growths that may resolve on their own but can be treated with therapies like salicylic acid. SA, a low-cost and effective over-the-counter option at concentrations ranging from 10-60%, removes infected skin layers but requires weeks of consistent use and careful dosing, especially in children, to avoid toxicity.
Ichthyosis
Ichthyosis is a genetic skin condition causing dry, thick, scaly skin. Treatments like salicylic acid, lactic acid, and urea-based creams can help soften and remove scales, even in newborns. However, careful dosing is crucial to avoid toxicity, especially in infants with more permeable skin.
I hope you enjoyed learning a bit about this important plant-derived medicine!
Yours in health, Dr. Quave
Cassandra L. Quave, Ph.D. is a Guggenheim Fellow, CNN Champion for Change, Fellow of the National Academy of Inventors, recipient of The National Academies Award for Excellence in Science Communication, and award-winning author of The Plant Hunter. Her day job is as professor and herbarium curator at Emory University School of Medicine, where she leads a group of research scientists studying medicinal plants to find new life-saving drugs from nature. She hosts the Foodie Pharmacology podcast and writes the Nature’s Pharmacy newsletter to share the science behind natural medicines. To support her effort, consider a paid or founding subscription to Nature’s Pharmacy or donation to her lab research.
Available in hardcover, paperback, audio, and e-book formats!